Coronavirus
What is Coronavirus?
Human coronaviruses are common across the world. First identified in the 1960s, human coronaviruses are a group of viruses that cause illnesses that can be mild, like a common cold, or severe, like Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV).
Coronaviruses are common in a variety of animal species such as bats and camels. While it is rare for coronaviruses to mutate, becoming zoonotic and infecting, then spreading between humans. Recent examples of these zoonotic viruses are SARS-CoV and MERS-CoV.
COVID-19 At-Home Tests
Each of the 13 NCHD county health departments offer free over the counter at-home test kits. Visit your local health department to request kits. The tests, also called over-the-counter tests or self-tests, can be taken anywhere. These rapid antigen tests give results in just a few minutes and do not need to be dropped off at a laboratory. PLEASE NOTE: these tests are for personal use and are not considered confirmed cases if the individual tests positive. We encourage anyone that tests positive using an at-home test to get confirmatory PCR testing.
COVID-19 Vaccine
For information on COVID-19 vaccine, including details on vaccine eligibility, safety, provider information, frequently asked questions and more, visit the NCHD COVID-19 vaccine page.
Healthcare providers who suspect COVID-19 infection in a patient should report them immediately to DPH by calling
1-866-PUB-HLTH (1-866-782-4584) and ask for a Medical Epidemiologist.
COVID-19 Data Resources
Get the latest COVID-19 data using the following resources:
- Georgia DPH COVID-19 Status Report
- DPH County Indicator Reports
- DPH COVID-19 Age Trends
- DPH Long Term Care Facility COVID-19 Weekly Summary
- Georgia Hospital Beds and Ventilator Use
- Georgia Medical Facility Patient Census
- Georgia COVID-19 Geospatial Data Hub
- CDC COVID-19 Data Tracker
- CDC COVID-19 County Check
- CDC COVID-19 Community Levels
- WHO COVID-19 Situation Reports
North Central Health District’s (NCHD) epidemiology program has shared COVID-19 Operations Summaries covering our 13-county district with media and the community. Reporting began April 17, 2020, and the final report was published Feb. 28, 2022. For the latest COVID-19 data, please use the links in our COVID-19 Data Resource Guide.
- April 2020 – Reports 1 & 2
- May 2020 – Reports 3-7
- June 2020 – Reports 8-12
- July 2020 – Special Report & Reports 13-16
- August 2020 – Reports 17-21
- September 2020 – Reports 22-25
- October 2020 – Reports 26-29
- November 2020 – Reports 30-34
- December 2020 – Reports 35-38
- January 2021 – Reports 39-42
- February 2021 – Reports 43-46
- March 2021 – Reports 47-51
- April 2021 – Reports 51-55
- May 2021 – Reports 56-60
- June 2021 – Reports 61 & 62
- July 2021 – Reports 63-64 & Special Report
- August 2021 – Reports 65-67
- September 2021 – Reports 68 & 69
- October 2021 – Reports 70 & 71
- November 2021 – Reports 72 & 73
- December 2021 – Reports 74 & 75
- January 2021 – Reports 76-78
- Report 79 – February 14, 2022
- Report 80 – February 28, 2022 – Final Report
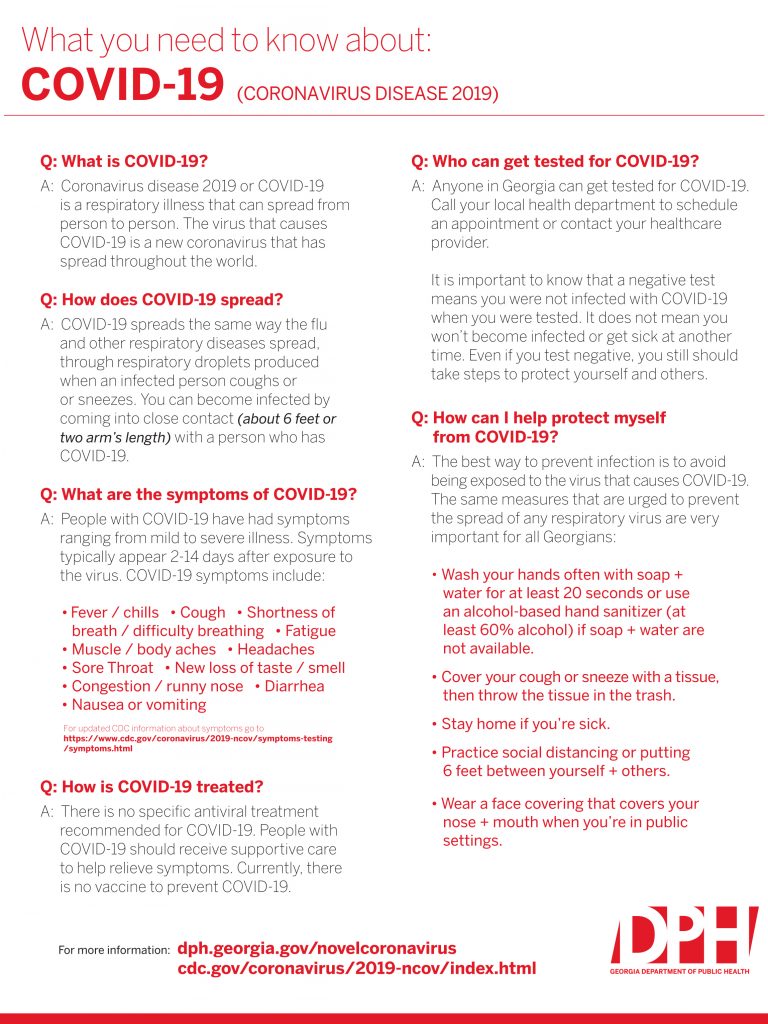
Methods of Transmission
Human coronaviruses are spread in ways similar to other viruses like the flu or norovirus. Common methods of transmission include:
- coughing
- sneezing
- close personal contact (shaking hands, touching, etc.)
- touching a contaminated object or surface, then touching your eyes, nose or mouth
- handling waste of an infected person (this method is rare)
Coronaviruses are commonly spread during fall and winter, but they are active all year.
Symptoms
Symptoms
COVID-19 can cause mild to severe symptoms and death. Symptoms may appear 2 to 14 days after exposure to the virus. Symptoms are similar to a variety of illnesses and include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Muscle pain
- Headache
- Sore throat
- New loss of taste or smell
- Congestion or runny nose
- Nausea
- Vomiting
- Diarrhea
The virus may lead to lower respiratory tract illnesses like pneumonia or bronchitis. This is more common in older adults, infants, people with compromised immune systems and people living with chronic conditions. Always contact your healthcare provider if symptoms persist or become more severe.
If you develop any of the following emergency warning signs, seek medical attention immediately:
- Trouble breathing
- Persistent chest pressure or pain
- New confusion
- Inability to wake or stay awake
- Bluish lips or face
Protection & Prevention
Protect Yourself
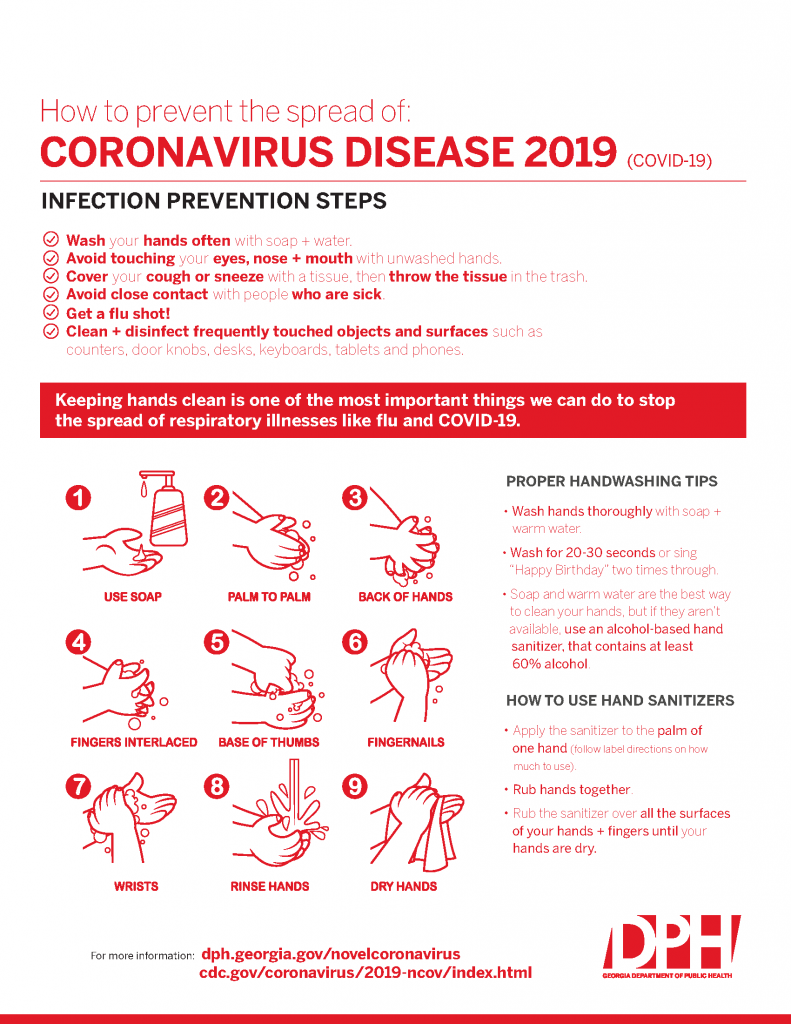
You can take steps to protect against the virus:
- Wash hands often with soap and hot water; wash hands for at least 20 seconds, especially after going to the bathroom, before eating and after blowing your nose, coughing or sneezing.
- If soap and water are unavailable, use an alcohol-based sanitizer with at least 60% alcohol.
- Avoid touching your eyes, nose or mouth.
- Avoid contact with people who are ill.
- Get vaccinated against COVID-19.
Protect Others
You can help reduce the risk of human coronavirus transmission. If you have cold-like symptoms:
- Stay home while you are sick.
- Avoid close contact with other people.
- Cover your nose and mouth when coughing and sneezing.
- Wash hands regularly.
- Disinfect surfaces and objects.
- Get vaccinated against COVID-19.
Avoid Travel to Active COVID-19 Areas
It is recommended to practice enhanced precautions if you are travelling to active COVID-19 areas, especially for older adults, infants and those with comporomised immune systems.
Basic Information for Schools
As a school administrator, there are steps you can take now to lessen the impact of a severe infectious disease outbreak in your school. It is important to review your health policies and emergency plans to ensure you’re prepared if COVID-19 infections begin to spread in our community.
The Centers for Disease Control & Prevention (CDC) is developing specific guidance for schools in response to COVID-19. Coronavirus is a respiratory illness that causes symptoms similar to influenza and is thought to be spread in the same way. The following strategies to prepare for a flu pandemic are a good starting point for your COVID-19 planning.
Create a Culture of Health in Your School
- Always promote healthy hygiene habits. Make sure students and staff have access to warm water and soap or hand sanitizer with at least 60% alcohol, tissues, and trash baskets. *Small children should only use hand sanitizer under adult supervision.
- Remind parents to keep sick children at home. Students should be symptom-free and fever-free for at least 24 hours without the use of fever-reducing medicines before returning to school.
- Also encourage staff to stay home when they’re sick. The same rules apply – employees should be symptom-free and fever-free for at least 24 hours before returning to school.
- Follow your standard procedures for routine cleaning and disinfecting. Typically, this means daily sanitizing surfaces and objects that are touched often, such as desks, countertops, doorknobs, computer keyboards, hands-on learning items, faucet handles, phones, and toys.
Planning Ahead
- Plan for staff and student absences. Develop flexible attendance and sick-leave policies that you can enact in a severe outbreak. Staff may need to stay home when they are sick, caring for a sick household member, or caring for their children in the event of school dismissals.
- Review your process for planning school events. Identify actions to take if you need to postpone or cancel events, such as sporting and special events.
- Identify space that can be used to separate sick people if possible. If an employee or student gets sick at school and cannot leave immediately, designate a separate area just for sick people if possible.
- Consider how you will handle school dismissals if public health recommends temporary school closures to lessen the spread of illness.
- Colleges and universities should also identify strategies to continue essential student services like meals, health, and social services. These plans should address students who are not able to return home, like international and out-of-state students.
Discourage Stigma & Discrimination
It’s also important to be mindful of the language you use and the policies you enact, ensuring you do not inadvertently promote stigma and discrimination. Do not make determinations of risk based on race or country of origin and be sure to maintain confidentiality of people with confirmed coronavirus infection.
CDC Interim Guidance for Schools
Guidance for K-12 Schools and School Based Programs
Return to School or Childcare Guidance After COVID-19 Illness or Exposure – Updated Jan. 6, 2021
Basic Information for Businesses
As an employer, there are steps you can take now to lessen the impact of an infectious disease outbreak on your workforce while ensuring your business operations can continue.
One of the most important things you can do is also one of the simplest: remind your staff that all sick employees should stay home and away from the workplace. Additionally, encourage employees to wash hands frequently, and ensure commonly touched surfaces are cleaned regularly.
Employees & Illness; Sick Leave
- Actively encourage sick employees to stay home. Employees should be symptom-free and fever-free for at least 24 hours without the use of fever-reducing medicines before returning to work.
- Ensure that your sick leave policies are flexible and consistent with public health guidance and that employees are aware of these policies.
- Talk with companies that provide your business with contract or temporary employees about the importance of sick employees staying home and encourage them to develop non-punitive leave policies.
- Do not require a healthcare provider’s note for employees who are sick with acute respiratory illness to validate their illness or to return to work, as healthcare provider offices and medical facilities may be extremely busy and not able to provide such documentation in a timely way.
- Employers should maintain flexible policies that permit employees to stay home to care for a sick family member. Employers should be aware that more employees may need to stay at home to care for sick children or other sick family members than is usual.
Encourage Healthy Behaviors
- Place posters that encourage staying home when sick, cough and sneeze etiquette, and hand hygiene at the entrance to your workplace and in other workplace areas where they are likely to be seen.
- Provide tissues and no-touch disposal receptacles for use by employees.
- Instruct employees to clean their hands often with an alcohol-based hand sanitizer that contains at least 60-95% alcohol or wash their hands with soap and water for at least 20 seconds. Soap and water should be used preferentially if hands are visibly dirty.
- Provide soap and water and alcohol-based hand rubs in the workplace. Ensure that adequate supplies are maintained. Place hand rubs in multiple locations or in conference rooms to encourage hand hygiene.
- Routinely clean all frequently touched surfaces in the workplace, such as workstations, countertops, and doorknobs. Use the cleaning agents that are usually used in these areas and follow the directions on the label.
Discourage Stigma & Discrimination
It’s also important to be mindful of the language you use and the policies you enact, ensuring you do not inadvertently promote stigma and discrimination in the workplace. Do not make determinations of risk based on race or country of origin and be sure to maintain confidentiality of people with confirmed coronavirus infection.
Return to Work Guidance for Non-Healthcare – Updated Dec. 4
Return to Work Guidance for Healthcare – Updated Dec. 4
COVID-19 FAQs
COVID-19 & Masks
CDC recommends wearing cloth face coverings in public where social distancing may be difficult to maintain (e.g., grocery stores and pharmacies). The use of simple cloth face coverings may help people who may have the virus and do not know it, from transmitting it to others. These cloth face coverings (made from household items like T-shirts, bandanas) can be used as an additional public health measure. It is important to note that the cloth face coverings recommended by the CDC are NOT surgical masks or N-95 respirators. Those items should continue to be reserved for healthcare workers and first responders, as recommended by current CDC guidance.
Guidance Documents:
- Georgia Department of Public Health
- Get the latest from DPH at the DPH COVID-19 Guidance Page.
- Environmental Protection Agency
- Food & Drug Administration
- Centers for Disease Control & Prevention:
Learn about our related health services:
Additional Resources


 Contact Us
Contact Us Locations
Locations Job Openings at North Central Health District
Job Openings at North Central Health District Internships
Internships Board of Health
Board of Health Cost and Insurance
Cost and Insurance Privacy Policy
Privacy Policy Teens & Adults
Teens & Adults For Children
For Children Other Programs
Other Programs County Environmental Health Offices
County Environmental Health Offices Chemical Hazards
Chemical Hazards Tourist Accommodations
Tourist Accommodations Food Service
Food Service Rabies Control
Rabies Control Lead Poisoning Prevention
Lead Poisoning Prevention Body Art
Body Art Land Use
Land Use Swimming Pool Program
Swimming Pool Program Water Testing for Private Wells
Water Testing for Private Wells Environmental Health Complaints
Environmental Health Complaints Georgia Food Recall Alerts
Georgia Food Recall Alerts Personal & Family Preparedness
Personal & Family Preparedness Emergency Preparedness for Functional & Access Needs
Emergency Preparedness for Functional & Access Needs Severe Weather Preparedness
Severe Weather Preparedness Emergency Preparedness Training
Emergency Preparedness Training Medical Reserve Corps
Medical Reserve Corps Regional Healthcare Coalitions
Regional Healthcare Coalitions Strategic National Stockpile/Medical Countermeasures
Strategic National Stockpile/Medical Countermeasures

